Feeling under the weather? Is it a common cold, the flu, or could it be COVID-19? With overlapping symptoms, it's understandable to be confused. Let's break down the key differences to help you understand what might be going on with your body.
The uncertainty surrounding illness can be overwhelming. Do you need to isolate? Are you contagious? Should you seek medical attention? Navigating these questions while feeling unwell adds to the stress.
This article aims to clarify the distinctions between the flu and COVID-19. We'll explore their symptoms, transmission methods, and potential complications, providing you with the knowledge to make informed decisions about your health.
In essence, this discussion emphasizes the nuances of differentiating the flu from COVID-19, highlighting symptom variations, modes of transmission, and possible health consequences. Understanding these disparities is crucial for informed decision-making regarding personal health and preventative measures. Core keywords include: flu, COVID-19, symptoms, transmission, differentiation, health, and prevention.
Symptom Overlap and Key Differences
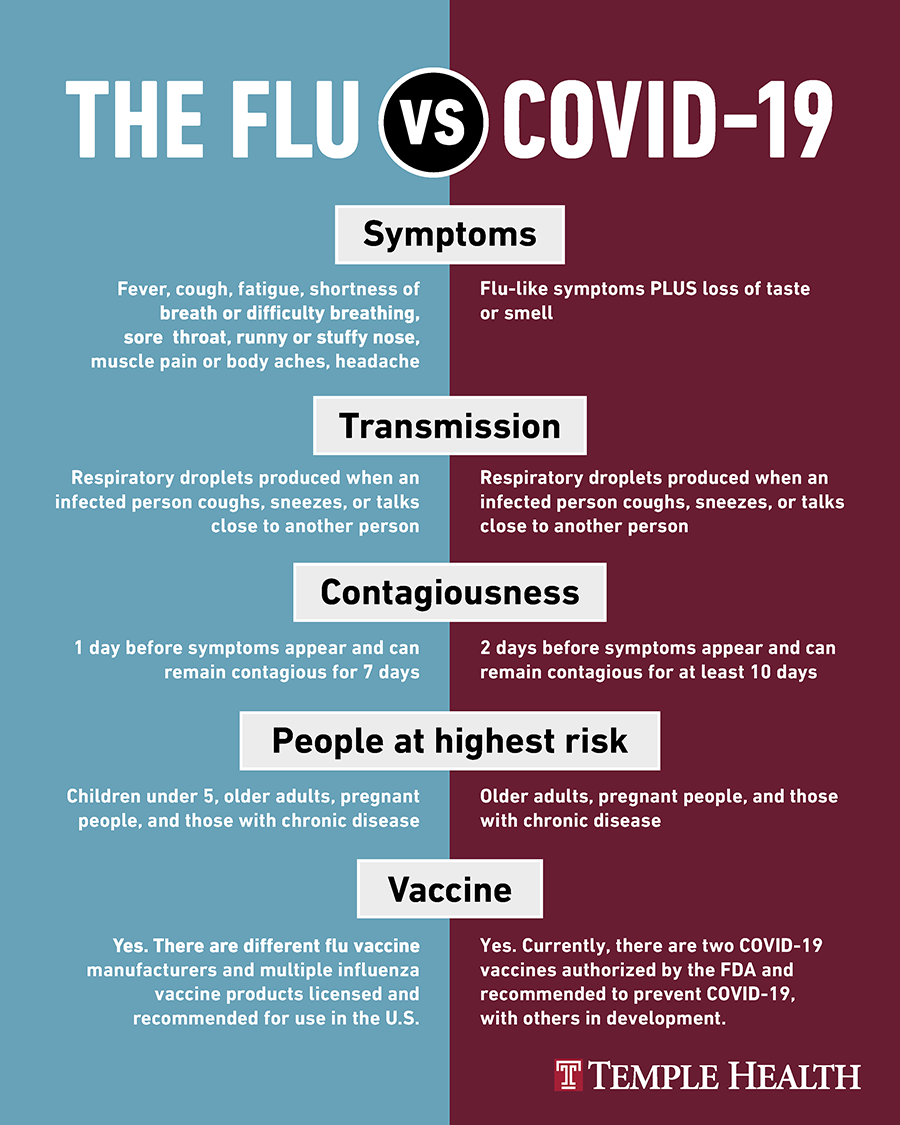
The goal here is to highlight the overlapping and distinct symptoms of the flu and COVID-19, guiding readers toward recognizing subtle cues that may indicate which illness they're experiencing. This knowledge empowers them to seek appropriate testing and care. I remember one time I had a really bad cough, and I just assumed it was a cold. I went to work for a few days, spreading germs around like it was my job. Turns out, it was the flu, and several of my colleagues got sick because of my carelessness! Since then, I've become much more cautious about respiratory symptoms. One of the biggest overlaps between the flu and COVID-19 is the presence of fever, cough, fatigue, and body aches. Both can leave you feeling drained and miserable. However, there are some key differences to watch out for. A sudden loss of taste or smell is more characteristic of COVID-19, although it can sometimes occur with a severe flu. Shortness of breath is also more common and tends to be more pronounced with COVID-19. While the flu can cause respiratory distress, it's generally less severe. Think about the severity of your symptoms and how quickly they came on. COVID-19 can sometimes have a slower onset, while the flu often hits you like a ton of bricks.
Transmission and Prevention
This section will explore how both illnesses spread, stressing the importance of hygiene practices and vaccination for prevention. Understanding these mechanisms helps individuals make informed choices to protect themselves and others. Both the flu and COVID-19 are respiratory illnesses, meaning they spread through droplets produced when an infected person coughs, sneezes, talks, or sings. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. The best way to prevent the spread of either illness is to practice good hygiene. Wash your hands frequently with soap and water for at least 20 seconds, especially after being in public places or touching surfaces that may be contaminated. Avoid touching your face, as this can transfer viruses from your hands to your respiratory system. Cover your coughs and sneezes with a tissue or your elbow. Vaccination is another crucial prevention strategy. Annual flu shots are highly recommended for everyone six months and older. While the effectiveness of the flu vaccine can vary depending on the strains circulating each year, it still offers significant protection against severe illness. Vaccines for COVID-19 are also available and highly effective in preventing infection, hospitalization, and death. Staying up-to-date on your vaccinations is one of the best ways to safeguard your health and protect your community.
Historical Context and Misconceptions
This will delve into the historical context of both illnesses, dispelling common myths and promoting accurate understanding based on scientific evidence. Addressing misinformation empowers readers to make informed health decisions. Throughout history, influenza outbreaks have caused widespread illness and death. The 1918 Spanish flu pandemic was particularly devastating, killing an estimated 50 million people worldwide. This historical context highlights the importance of taking respiratory illnesses seriously and implementing preventative measures. COVID-19, a novel virus, emerged in late 2019 and quickly spread across the globe, causing a global pandemic. The rapid transmission and severity of the illness led to widespread lockdowns and significant disruptions to daily life. Many misconceptions surround both the flu and COVID-19. One common myth is that the flu is just a bad cold. While both illnesses can cause similar symptoms, the flu is generally more severe and can lead to serious complications, such as pneumonia and hospitalization. Another misconception is that the COVID-19 vaccine is ineffective. Studies have consistently shown that the vaccines are highly effective in preventing severe illness, hospitalization, and death, even against emerging variants. Relying on accurate information from reputable sources, such as the CDC and WHO, is crucial for dispelling myths and making informed decisions about your health.
Hidden Dangers and Potential Complications
This section will uncover the hidden dangers associated with both the flu and COVID-19, emphasizing the potential for serious complications, especially in vulnerable populations. Raising awareness of these risks encourages proactive health management. While most people who get the flu or COVID-19 recover without complications, both illnesses can lead to serious health problems, especially in vulnerable populations. The flu can cause pneumonia, bronchitis, sinus infections, and ear infections. In some cases, it can also lead to more severe complications, such as heart inflammation and brain inflammation. COVID-19 can also cause pneumonia, bronchitis, and blood clots. In some cases, it can lead to acute respiratory distress syndrome (ARDS), a life-threatening condition that requires hospitalization. People with underlying health conditions, such as asthma, diabetes, and heart disease, are at higher risk of developing serious complications from both the flu and COVID-19. Pregnant women, older adults, and young children are also at increased risk. If you are at high risk of complications, it's especially important to get vaccinated against both the flu and COVID-19 and to seek medical attention if you develop symptoms. Early diagnosis and treatment can help prevent serious complications and improve your chances of recovery.
Recommendations for Managing Symptoms and Seeking Care
Here, we'll provide actionable recommendations for managing symptoms at home and guidance on when to seek professional medical care, ensuring readers are equipped to handle illness effectively. When you're feeling under the weather with flu-like or COVID-like symptoms, there are several things you can do to manage your symptoms at home. Get plenty of rest and drink lots of fluids to stay hydrated. Over-the-counter medications, such as pain relievers and decongestants, can help alleviate symptoms like fever, body aches, and congestion. If you have a cough, consider using a cough suppressant or expectorant to help loosen mucus. It's also important to isolate yourself from others to prevent the spread of infection. Stay home from work or school and avoid close contact with family members. However, it's important to know when to seek medical care. If you experience severe symptoms, such as difficulty breathing, chest pain, persistent dizziness, or confusion, seek immediate medical attention. If you have underlying health conditions or are at high risk of complications, it's also important to consult with your doctor. They may recommend antiviral medications, which can help shorten the duration of the illness and reduce the risk of complications. Remember, early diagnosis and treatment are crucial for preventing serious health problems.
The Role of Testing and Diagnosis
This section dives into the importance of testing and accurate diagnosis in differentiating between the flu and COVID-19, highlighting the available testing options and their implications. Testing is a crucial tool for differentiating between the flu and COVID-19. While the symptoms can overlap, knowing which virus you have is essential for making informed decisions about your health and preventing the spread of infection. Several types of tests are available for both the flu and COVID-19. Rapid antigen tests can provide results in as little as 15 minutes, but they are generally less sensitive than PCR tests. PCR tests are more accurate but take longer to process. Both types of tests involve collecting a sample from your nose or throat using a swab. If you are experiencing symptoms of the flu or COVID-19, it's important to get tested as soon as possible. Early diagnosis allows you to start treatment promptly and take steps to prevent the spread of infection to others. If you test positive for the flu or COVID-19, follow your doctor's recommendations for treatment and self-isolation. If you test negative but continue to experience symptoms, it's important to stay home and monitor your condition. You may need to get retested, especially if you have been exposed to someone with the virus. Regular testing, especially for those who are at high risk, is very important.
Practical Tips for Staying Healthy During Respiratory Virus Season
This section will offer actionable tips for maintaining optimal health during peak seasons for respiratory viruses, empowering readers to proactively protect themselves from illness. During respiratory virus season, there are several practical steps you can take to protect yourself and others. Start by practicing good hygiene. Wash your hands frequently with soap and water, avoid touching your face, and cover your coughs and sneezes. Consider wearing a mask in public places, especially if you are in crowded indoor settings. Masks can help prevent the spread of respiratory droplets and protect you from inhaling the virus. Boost your immune system by getting enough sleep, eating a healthy diet, and exercising regularly. A strong immune system can help you fight off infections more effectively. Avoid close contact with people who are sick. If you know someone who has the flu or COVID-19, stay away from them to prevent getting infected. Disinfect frequently touched surfaces, such as doorknobs, countertops, and phones. Viruses can live on surfaces for hours, so regular cleaning can help reduce the risk of transmission. Stay informed about the latest recommendations from public health officials. The CDC and WHO provide up-to-date information on the flu and COVID-19, including vaccination recommendations and prevention guidelines. By following these tips, you can significantly reduce your risk of getting sick during respiratory virus season.
The Importance of Mental Well-being During Illness
This section will address the often-overlooked aspect of mental health during illness, offering strategies for managing stress, anxiety, and isolation while recovering from the flu or COVID-19. Being sick can take a toll on your mental health. The symptoms of the flu and COVID-19 can be physically and emotionally draining. It's important to prioritize your mental well-being during illness. Acknowledge your feelings. It's okay to feel stressed, anxious, or frustrated when you're sick. Don't try to suppress your emotions. Talk to someone you trust. Sharing your feelings with a friend, family member, or therapist can help you cope with the emotional challenges of being sick. Practice self-care. Do things that make you feel good, such as reading a book, watching a movie, or taking a relaxing bath. Limit your exposure to news and social media. Constant updates about the pandemic can increase anxiety and stress. Stay connected with others. If you're isolating, use technology to stay in touch with friends and family. Virtual connections can help you feel less lonely and isolated. Get enough rest. Sleep is essential for both physical and mental recovery. Don't push yourself to do too much when you're sick. If you're struggling with your mental health, don't hesitate to seek professional help. A therapist or counselor can provide you with support and coping strategies.
Fun Facts About the Flu and COVID-19
This section will present interesting and lesser-known facts about the flu and COVID-19, engaging readers with captivating information while reinforcing key concepts. Did you know that the flu virus is constantly changing? This is why you need to get a new flu shot every year. The virus mutates, so last year's vaccine may not be effective against this year's strains. COVID-19 is caused by a novel coronavirus, meaning it's a new strain that humans haven't been exposed to before. This is why it spread so rapidly and caused a global pandemic. The flu has been around for centuries. The earliest recorded influenza pandemic was in 1580. COVID-19 is much newer, but it has already had a significant impact on the world. Both the flu and COVID-19 can affect animals. Birds, pigs, and other animals can get the flu, and some animals can also get COVID-19. The symptoms of the flu and COVID-19 can vary from person to person. Some people experience mild symptoms, while others get very sick. The best way to protect yourself from the flu and COVID-19 is to get vaccinated. Vaccines are safe and effective and can help prevent severe illness. Researchers are constantly learning more about the flu and COVID-19. New treatments and prevention strategies are being developed all the time. Staying informed about the latest scientific advancements can help you make informed decisions about your health.
How to Boost Your Immune System to Fight Off Illness
This section will provide practical strategies for strengthening the immune system, empowering readers to proactively defend against the flu, COVID-19, and other infections. A strong immune system is essential for fighting off infections. There are several things you can do to boost your immune system naturally. Eat a healthy diet. Focus on fruits, vegetables, whole grains, and lean protein. Avoid processed foods, sugary drinks, and excessive amounts of alcohol. Get enough sleep. Aim for 7-8 hours of sleep per night. Sleep deprivation can weaken your immune system. Exercise regularly. Physical activity helps boost your immune cells and improve your overall health. Manage stress. Chronic stress can suppress your immune system. Find healthy ways to manage stress, such as yoga, meditation, or spending time in nature. Take vitamin and mineral supplements. Vitamin C, vitamin D, and zinc are essential for immune function. Consider taking supplements if you're not getting enough of these nutrients from your diet. Stay hydrated. Drink plenty of water to keep your body functioning properly. Avoid smoking. Smoking damages your immune system and increases your risk of infection. By following these tips, you can strengthen your immune system and reduce your risk of getting sick. Remember, a healthy lifestyle is the best defense against illness.
What If You Experience Long-Term Symptoms After Flu or COVID-19?
This section will address the possibility of long-term health issues following a flu or COVID-19 infection, providing guidance on seeking appropriate medical care and support. Some people experience long-term symptoms after recovering from the flu or COVID-19. These symptoms can persist for weeks or months and can significantly impact your quality of life. Long-term symptoms after the flu are sometimes referred to as "post-influenza syndrome." This can include fatigue, cough, and difficulty concentrating. Long-term symptoms after COVID-19 are sometimes referred to as "long COVID." This can include a wide range of symptoms, such as fatigue, shortness of breath, brain fog, muscle aches, and loss of taste or smell. If you experience long-term symptoms after the flu or COVID-19, it's important to seek medical attention. Your doctor can evaluate your condition and recommend appropriate treatment. There is no one-size-fits-all treatment for long-term symptoms. Treatment may involve medication, physical therapy, occupational therapy, or mental health counseling. It's also important to manage your symptoms at home. Get plenty of rest, eat a healthy diet, and avoid overexertion. Joining a support group can also be helpful. Connecting with other people who are experiencing long-term symptoms can provide emotional support and practical advice. Remember, you're not alone. Many people are experiencing long-term symptoms after the flu or COVID-19, and there is hope for recovery.
Listicle: Top 5 Things to Remember About Flu vs. COVID-19
This section presents a concise and memorable list of key takeaways, reinforcing the most important information for readers to remember. 1. Symptoms can overlap: Both the flu and COVID-19 can cause fever, cough, fatigue, and body aches.
2. Loss of taste or smell is more common with COVID-19: This symptom is less frequently seen with the flu.
3. Testing is essential: Get tested to confirm your diagnosis and guide treatment decisions.
4. Prevention is key: Get vaccinated, practice good hygiene, and avoid close contact with sick people.
5. Seek medical attention for severe symptoms: Don't hesitate to consult a doctor if you experience difficulty breathing, chest pain, or persistent dizziness.
Question and Answer
Q: How can I tell if I have the flu or COVID-19 without getting tested?
A: It's difficult to definitively distinguish between the flu and COVID-19 based on symptoms alone. A loss of taste or smell is more suggestive of COVID-19, but the best way to know for sure is to get tested.
Q: Are there different treatments for the flu and COVID-19?
A: Yes. Antiviral medications are available for both the flu and COVID-19, but they are different drugs. Your doctor can determine the appropriate treatment based on your diagnosis.
Q: If I had COVID-19 already, do I still need to get a flu shot?
A: Yes. COVID-19 and the flu are different viruses, and having immunity to one does not protect you from the other. Getting a flu shot is still recommended.
Q: What should I do if I think I have either the flu or COVID-19?
A: Stay home, isolate yourself from others, and get tested as soon as possible. Consult with your doctor about treatment options.
Conclusion of Health Flu vs. COVID-19: Know the Crucial Differences!
Understanding the differences between the flu and COVID-19 is essential for protecting your health and the health of those around you. While symptoms can overlap, key distinctions exist, and testing is crucial for accurate diagnosis. By practicing good hygiene, staying up-to-date on vaccinations, and seeking medical attention when needed, you can navigate respiratory virus season with confidence and take proactive steps to safeguard your well-being.